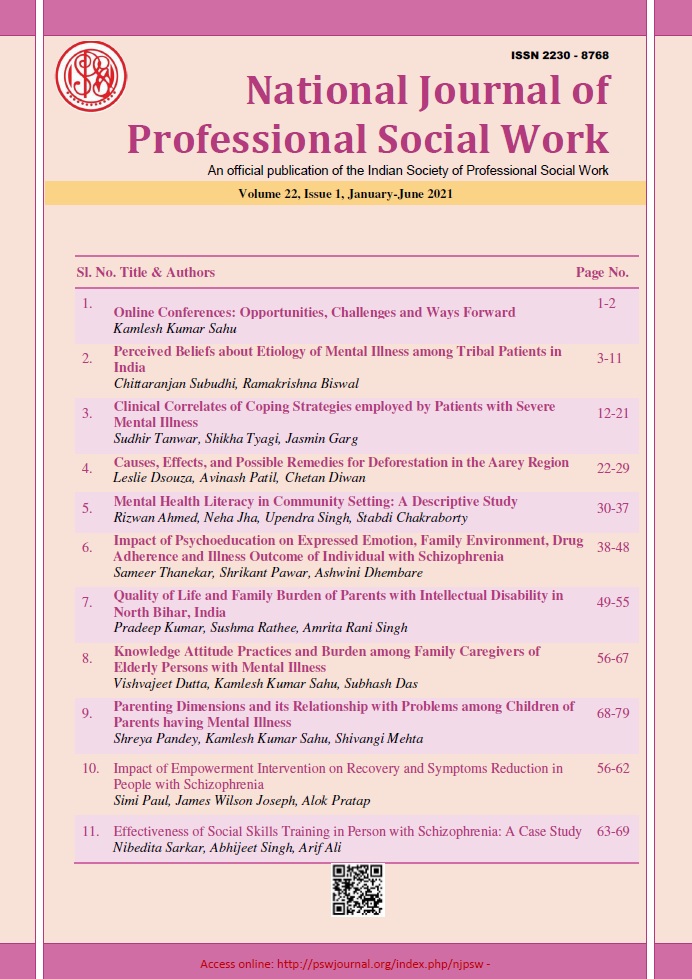
Impact of Psychoeducation on Expressed Emotion, Family Environment, Drug Adherence and Illness Outcome of Individual with Schizophrenia
DOI:
https://doi.org/10.51333/njpsw.2021.v22.i1.292Abstract
Background: Psychoeducation can be implemented in different formats and settings. The format depends entirely on the disorder, the developmental age of the individual, and their individual needs. Individual-based, Family-based, Group-based. Psycho-education most commonly involves the individual with the disorder, the patient or client, but in some situations, psychoeducation is implemented only to the people who deal with the patient on a day-to-day basis such as family, friends, teachers, or caretakers. Aim: To assess the impact of psychoeducation on expressed emotion, family environment, drug adherence, and illness outcome of the individual with schizophrenia. Methodology: It will be a hospital-based intervention study using pre-post-test control group research design. This study has been conducted to evaluate the efficacy of psychoeducation on different outcome variables. Results: After the intervention, it was found that family environment and drug adherence improved and expressed emotions reduced. So in schizophrenia role of psychoeducation is important. its improved family environment reduced expressed emotions and improved drug adherence.
Keywords: Medication adherence, family environment, attitude
References
Anderson, C. M., Reiss, D. J. & Hogarty, G. E. (1986). Schizophrenia and the family. A practitioner’s guide to psychoeducation and management. New York: Guilford Press
Amaresha, A. C., & Venkatasubramanian, G. (2012). Expressed emotion in schizophrenia: an overview. Indian Journal of Psychological Medicine, 34(1), 12-20.
Ascher-Svanum, H., Zhu, B., Faries, D., Lacro, J. P., & Dolder, C. R. (2006). A prospective study of risk factors for nonadherence with antipsychotic medication in the treatment of schizophrenia. Journal of Clinical Psychiatry, 67(7), 1114-1123.
Awad, A. G. (2004). Antipsychotic medications: compliance and attitudes towards treatment. Current Opinion in Psychiatry, 17(2), 75-80.
Banerjee, A. G., & Retamero, C.. Expressed emotions-a determinant of relapse in schizophrenia: a case report and literature review. Journal of Psychiatry and Brain Functions, 2014, 1, 4. http://dx.doi.org/10.7243/2055-3447-1-4
Barkhof, E., Meijer, C. J., de Sonneville, L. M., Linszen, D. H., & de Haan, L. (2012). Interventions to improve adherence to antipsychotic medication in patients with schizophrenia–a review of the past decade. European Psychiatry, 27(1), 9-18.
Dolder, C. R., Lacro, J. P., Warren, K. A., Golshan, S., Perkins, D. O., & Jeste, D. V. (2004). Brief evaluation of medication influences and beliefs: development and testing of a brief scale for medication adherence. Journal of clinical psychopharmacology, 24(4), 404-409.
Pekkala, E. T., & Merinder, L. B. (2002). Psychoeducation for schizophrenia. Cochrane Database of Systematic Reviews, (2). https://doi.org/10.1002/14651858.CD002831
Haynes, R. B. Introduction. In: R. B. Haynes, D. W. Taylor, & D. L. Sackett, editors. Compliance in health care. Baltimore: John Hopkins University.
Hogan, T. P., Awad, A. G., & Eastwood, R. (1983). A self-report scale predictive of drug compliance in schizophrenics: reliability and discriminative validity. Psychological medicine, 13(1), 177-183.
Jeste, S. D., Patterson, T. L., Palmer, B. W., Dolder, C. R., Goldman, S., & Jeste, D. V. (2003). Cognitive predictors of medication adherence among middle-aged and older outpatients with schizophrenia. Schizophrenia Research, 63(1-2), 49-58.
Kane, J. M. (2007). Treatment adherence and long-term outcomes. CNS spectrums, 12(S17), 21-26.
Moos, R., & Moos, B. (1976). A typology of family social environments. Family Process, 15: 357-371.
Murali, T., Sudarshan, B. & Taly, A. B. (2001). Foundations and techniques in psychiatric rehabilitation. Manual for CBR workers and caregivers. Bangalore: National Institute of Mental Health and Neurosciences
Nirmala, B. P., Vranda, M. N., & Reddy, S. (2011). Expressed emotion and caregiver burden in patients with schizophrenia. Indian journal of psychological medicine, 33(2), 119-122.
Sethi, B. B., Chaturvedi, P. K., Saxena, N. K., & Trivedi, J. K. (1982). A Comparative Study of Attitudes of the Key Relatives towards ‘Schizophrenic Patients’ and ‘Patients of Disturbed Family’. Indian journal of psychiatry, 24(2), 126-130.
Shankar, R. & Menon, M. S. (1997). Working with families who look after an affected member with psychiatric disabilities. A training manual for mental health professionals. Chennai: Schizophrenia Research Foundation (India) & World Association of Psychosocial Rehabilitation (Indian Chapter)
Thompson, K., Kulkarni, J., & Sergejew, A. A. (2000). Reliability and validity of a new Medication Adherence Rating Scale (MARS) for the psychoses. Schizophrenia research, 42(3), 241-247.
World Health Organization. (1996). Psychosocial rehabilitation. A consensus statement. Geneva, World Health Organization.
Yamada, K., Watanabe, K., Nemoto, N., Fujita, H., Chikaraishi, C., Yamauchi, K., ... & Kanba, S. (2006). Prediction of medication noncompliance in outpatients with schizophrenia: 2-year follow-up study. Psychiatry Research, 141(1), 61-69.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2021 National Journal of Professional Social Work

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.