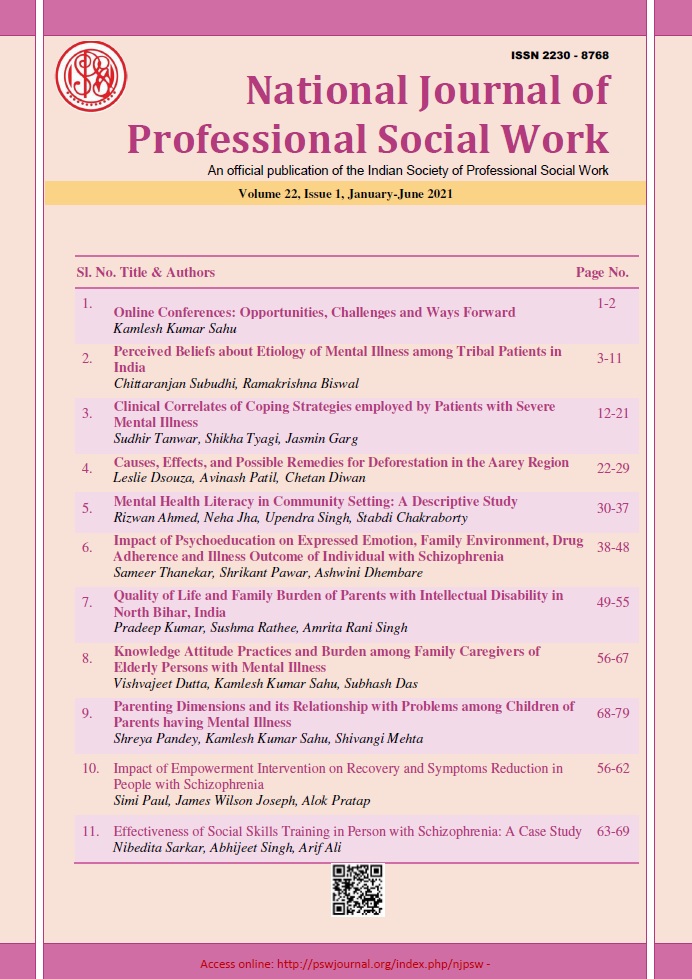
Mental Health Literacy in Community Setting: A Descriptive Study
DOI:
https://doi.org/10.51333/njpsw.2021.v22.i1.291Abstract
Background: Mental health literacy is important for all societies, it will be helpful for reducing the treatment gap. Mental health campaigns can reduce the chronic city of psychiatric disorders, illness can treat as earliest as possible. Community awareness of Psychiatric Disorders helps to reduce stigma, discrimination, sensitization, treatment and social inclusion. Aim: To assess the literacy level of Mental Illness among the community people. Methodology: The study was conducted at the rural health training centre, Najafgarh, Delhi. Simple survey methods were used for data collection. A total of 306 individuals were selected for the study. The researcher informs community people with help of ASHA workers to come to RHTC, Najafgarh. Participants were asked to complete a questionnaire that was designed specifically for Indian contexts and was translated into Hindi. Tools were used for the study Socio-demographic datasheet and the public perceptions of mental illness questionnaire applied which assess the area of the previous contact with people with mental health issues, understanding of the psychiatric disorder, knowledge of psychiatric illness and attitude towards the individual with mental problems. The questionnaire was translated into Hindi, and independently back-translated by research experts in the mental health field.
Results: Results show that the mean age of participants was 33 years, 62% participants male and 37% participants female. Participants understanding of mental health among the community participants negative perception was higher. Less mental Health services availability reported in the community. Conclusion: Mental health awareness is one of the most important phenomenon for increased literacy and reducing the treatment gap-related Mental Health.
Keywords: Mental Illness. Community, Awareness, Treatment Gap
References
Akighir, A. (1982). Traditional and modern psychiatry: a survey of opinions and beliefs amongst people in plateau state, Nigeria. International Journal of Social Psychiatry, 28(3), 203-209.
Angermeyer, M. C., & Matschinger, H. (1999). Lay beliefs about mental disorders: a comparison between the western and the eastern parts of Germany. Social Psychiatry and Psychiatric Epidemiology, 34(5), 275-281.
Adewuya, A. O., & Makanjuola, R. O. (2008). Lay beliefs regarding causes of mental illness in Nigeria: pattern and correlates. Social psychiatry and psychiatric epidemiology, 43(4), 336-341.
Angermeyer, M. C., Holzinger, A., & Matschinger, H. (2009). Mental health literacy and attitude towards people with mental illness: a trend analysis based on population surveys in the eastern part of Germany. European Psychiatry, 24(4), 225-232.
Bloom, D. E., Chisholm, D., Jané-Llopis, E., Prettner, K., Stein, A., & Feigl, A. (2011). From Burden to “Best Buys”: Reducing the Economic Impact of Non-Communicable Diseases. World Health Org., Geneva, Switzerland.
Fleischmann, A., & Saxena, S. (2013). Suicide prevention in the WHO Mental Health Gap Action Programme (mhGAP).
Furnham, A., & Swami, V. (2018). Mental health literacy: A review of what it is and why it matters. International Perspectives in Psychology, 7(4), 240-257.
Gaebel, W., Baumann, A., Witte, A. M., & Zaeske, H. (2002). Public attitudes towards people with mental illness in six German cities. European archives of psychiatry and clinical neuroscience, 252(6), 278-287.
Gureje, O. Y. E., Lasebikan, V. O., Ephraim-Oluwanuga, O., Olley, B. O., & Kola, L. (2005). Community study of knowledge of and attitude to mental illness in Nigeria. The British Journal of Psychiatry, 186(5), 436-441.
Hayward, P., & Bright, J. A. (1997). Stigma and mental illness: A review and critique. Journal of Mental Health, 6(4), 345-354.
Kermode, M., Bowen, K., Arole, S., Pathare, S., & Jorm, A. F. (2009). Attitudes to people with mental disorders: a mental health literacy survey in a rural area of Maharashtra, India. Social psychiatry and psychiatric epidemiology, 44(12), 1087-1096.
Logan, H., Guo, Y., Dodd, V. J., Muller, K., & Riley, J. (2013). The burden of chronic diseases in a rural North Florida sample. BMC public health, 13(1), 1-9.
Mojtabai, R., Olfson, M., & Mechanic, D. (2002). Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Archives of general psychiatry, 59(1), 77-84.
Paula, C. S., Lauridsen-Ribeiro, E., Wissow, L., Bordin, I. A., & Evans-Lacko, S. (2012). How to improve the mental health care of children and adolescents in Brazil: actions needed in the public sector. Brazilian Journal of Psychiatry, 34, 334-351.
Shibre, T., Negash, A., Kullgren, G., Kebede, D., Alem, A., Fekadu, A., ... & Jacobsson, L. (2001). Perception of stigma among family members of individuals with schizophrenia and major affective disorders in rural Ethiopia. Social Psychiatry and Psychiatric Epidemiology, 36(6), 299-303.
Stuart, H., & Arboleda-Florez, J. (2001). Community attitudes toward people with schizophrenia. The Canadian Journal of Psychiatry, 46(3), 245-252.
Weller, L., & Grunes, S. (1988). Does contact with the mentally ill affect nurses; attitudes to mental illness? British Journal of Medical Psychology, 61(3), 277-284.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2021 National Journal of Professional Social Work

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.