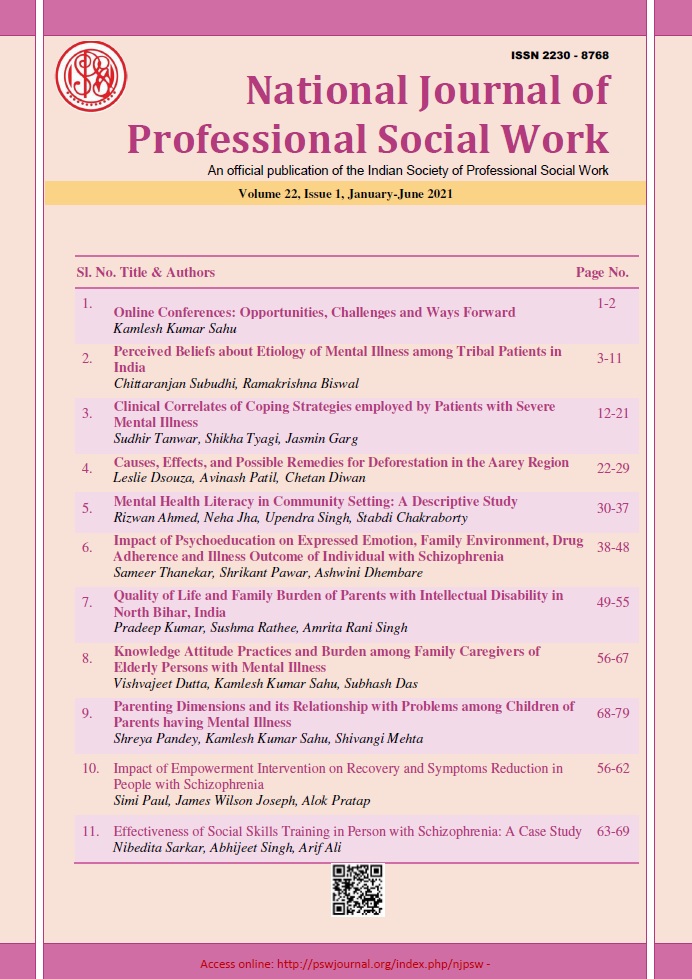
Clinical Correlates of Coping Strategies employed by Patients with Severe Mental Illness
DOI:
https://doi.org/10.51333/njpsw.2021.v22.i1.289Abstract
Background: Coping strategies are the behavioural and cognitive efforts directed to manage stressful demands of life. Coping is generally believed to be a constructive and adaptive effort, which an individual consciously employs to minimize or reduce stress. The aim of the study was to assess the coping strategies employed by patients with Severe Mental Illness (SMI) and evaluate the relationship between the level of insight, the severity of illness and socio-occupational functioning with coping strategies. Method: This cross-sectional study was conducted with 60 outpatients of SMI who were inducted from the rehabilitation subunit of the Department of Psychiatry of Government Medical College & Hospital, Sector 32, Chandigarh. Patients were assessed on Ways of Coping Checklist-Hindi Adaptation (WCC-HA), Brief Psychiatric Rating Scale (BPRS), Schedule for Assessment of Insight (SAI-E), Global Assessment of Functioning (GAF) and Socio-occupational Functioning Scale (SOFS). Results: On the WCC-HA scale, the mean score of seeking social support was10.48± 3.80, avoiding situation 15.11 ± 5.43 and problem-focused 5.03 ± 3.11. There was no significant difference between the types of coping employed by patients with SMI on ANOVA. Avoiding Situation strategies of coping shows a significant positive correlation (r = 0.465, p = 0.01) with the severity of illness (BPRS). Adaptive coping strategies showed a significant positive correlation [seeking social support (r = 0.430), and problem-focused (r = 0.546) both at p = 0.01] with insight of illness (SAI- E). No significant correlation was found between coping and socio-occupational functioning of patients of SMI. [avoiding situation (r =.239), seeking social support (r = .025), problem-focused (r = -.429)] Conclusion: Coping strategies of patients SMI varied with their levels of psychopathology and insight. Those with comparatively severe psychopathology and poorer insight tended to use avoidant or maladaptive coping strategies more often.
Keywords: severe mental illness, coping strategies, insight
References
American Psychiatric Association. (2014). Desk Reference to the diagnostic criteria from DSM-5®. American Psychiatric Publication.
Böker, W., Brenner, H. D., Gerstner, G., Keller, F., Müller, J., & Spichtig, L. (1984). Self‐healing strategies among schizophrenics: attempts at compensation for basic disorders. Acta Psychiatrica Scandinavica, 69(5), 373-378.
Boschi, S., Adams, R. E., Bromet, E. J., Lavelle, J. E., Everett, E., & Galambos, N. (2000). Coping with psychotic symptoms in the early phases of schizophrenia. American Journal of Orthopsychiatry, 70(2), 242-252.
Brazo, P., Dollfus, S., & Petit, M. (1995, August). Anti-hallucinatory coping strategies in schizophrenia. Annales Medico-Psychologiques. 153,456-9.
Breier, A., & Strauss, J. S. (1983). Self-control in psychotic disorders. Archives of general psychiatry, 40(10), 1141-1145.
Brenner, H. D., Böker, W., Müller, J., Spichtig, L., & Würgler, S. (1987). On autoprotective efforts of schizophrenics, neurotics and controls. Acta Psychiatrica Scandinavica, 75(4), 405-414.
Chadda, R. K., Singh, T. B., Ganguly, K. K. (2007). A prospective study of relationship between burden and coping in caregivers of patients with schizophrenia and bipolar affective disorder. Social Psychiatry and Psychiatric Epidemiology.42, 22-30.
David, AS. (1990). Insight and psychosis. The British Journal of Psychiatry, 156(6), 798-808
Falloon, I. R., & Talbot, R. E. (1981). Persistent auditory hallucinations: Coping mechanisms and implications for management. Psychological Medicine, 11(2), 329-339.
Folkman, S., & Lazarus, R. S. (1984). Stress, appraisal, and coping. New York: Springer Publishing Company.
Folkman S., Lazarus RS. (1985). If it changes it must be a process: a study of emotion and coping during three stages of a college examination. Journal of Personality and Social Psychology, 48, 150-170.
Frederick, J., & Cotanch, P. (1995). Self-help techniques for auditory hallucinations in schizophrenia. Issues in Mental Health Nursing, 16(3), 213-224.
Garcelán, S. P., & Rodríguez, A. G. (2002). Coping strategies in psychotics: conceptualization and research results. Psychology in Spain, 6(1), 26-40.
Heller, T., Roccoforte, J. A., Hsieh, K., Cook, J. A., & Pickett, S. A. (1997). Benefits of support groups for families of adults with severe mental illness. American Journal of Orthopsychiatry, 67(2), 187-198.
Holmes, E. P., & River, L. P. (1998). Individual strategies for coping with the stigma of severe mental illness. Cognitive and Behavioral Practice. 5(2), 231-239.
Lysaker, P. H., Bryson, G. J., Marks, K., Greig, T. C., & Bell, M. D. (2004). Coping style in schizophrenia: associations with neurocognitive deficits and personality. Schizophrenia Bulletin, 30(1), 113-121.
Lysaker, P. H., Roe, D., & Yanos, P. T. (2007). Toward understanding the insight paradox: internalized stigma moderates the association between insight and social functioning, hope, and self-esteem among people with schizophrenia spectrum disorders. Schizophrenia Bulletin, 33(1), 192-199.
Lysaker, P. H., Bryson, G. J., Lancaster, R. S., Evans, J. D., & Bell, M. D. (2003). Insight in schizophrenia: associations with executive function and coping style. Schizophrenia research, 59(1), 41-47.
Lysaker, P. H., Campbell, K., & Johannesen, J. K. (2005). Hope, awareness of illness, and coping in schizophrenia spectrum disorders: evidence of an interaction. The Journal of Nervous and Mental Disease, 193(5), 287-292.
Parabiaghi, A., Bonetto, C., Ruggeri, M., Lasalvia, A., & Leese, M. (2006). Severe and persistent mental illness: a useful definition for prioritizing community-based mental health service interventions. Social Psychiatry and Psychiatric Epidemiology, 41(6), 457-463.
Roe, D., Yanos, P. T., & Lysaker, P. H. (2006). Coping with psychosis: an integrative developmental framework. The Journal of Nervous and Mental Disease, 194(12), 917-924.
Saraswat, N., Rao, K., Subbakrishna, D. K., & Gangadhar, B. N. (2006). The Social Occupational Functioning Scale (SOFS): a brief measure of functional status in persons with schizophrenia. Schizophrenia Research, 81(2-3), 301-309.
Shah, R., Grover, S., & Kulhara, P. (2017). Coping in residual schizophrenia: Re-analysis of ways of coping checklist. The Indian Journal of Medical Research. 145(6), 786.
Van den Bosch R. J., Rombouts R. (1997) Coping and cognition in schizophrenia and depression. Compr Psychiatr, 38(6), 341-344.
Ventura, J., Lukoff, D., Nuechterlein, K. H., Liberman, R. P., Green, M., Shaner, A. (1993) Appendix 1: Brief Psychiatric Rating Scale (BPRS) expanded version (4.0) scales, anchor points and administration manual. International Journal of Methods in Psychiatric Research 3, 227–243.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2021 National Journal of Professional Social Work

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.